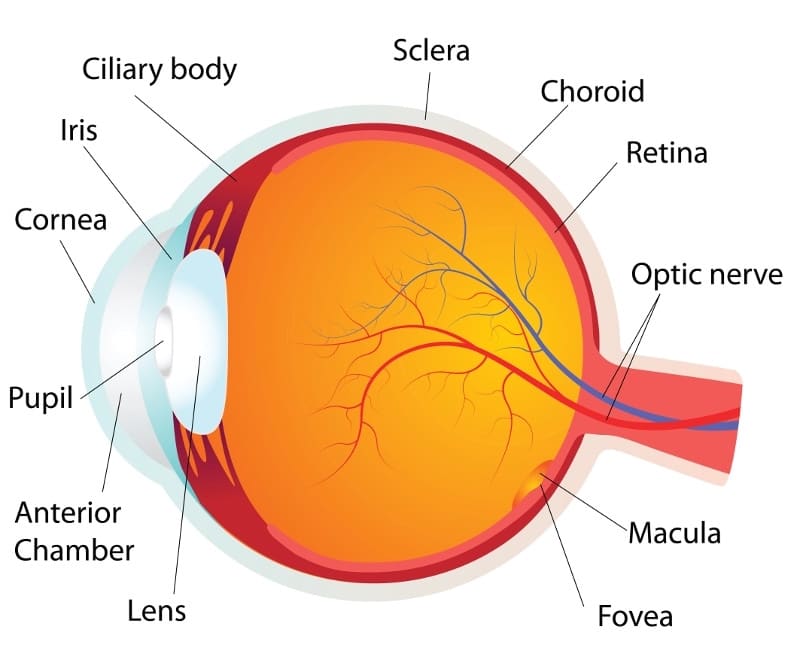
Clemson Eye’s Dr. Justin Roman specializes in treatment of cornea external diseases. The cornea is the clear, outer surface of your eye responsible for focusing power. If a cornea is damaged, the light that enters the eye is distorted causing the image you see to be blurry. A cornea may become damaged in several ways, including injury, disease, infection or previous eye surgery. Sometimes damage to the cornea is mild enough that it may be repaired to restore vision. If not, a corneal transplant may be necessary.
The most common allergies that affect the eye are those related to pollen, particularly when the weather is warm and dry. Symptoms in the eye include redness, itching, tearing, burning, stinging, and watery discharge, although usually not severe enough to require medical attention. Antihistamine decongestant eyedrops effectively reduce these symptoms. Rain and cooler weather, which decreases the amount of pollen in the air, can also provide relief.
Keratitis is an inflammation of the cornea. Noninfectious keratitis can be caused by a minor injury, or from wearing contact lenses too long. Infection is the most common cause of keratitis. Infectious keratitis can be caused by bacteria, viruses, fungi or parasites. Often, these infections are also related to contact lens wear, especially improper cleaning of contact lenses or overuse of old contact lenses that should be discarded. Minor corneal infections are usually treated with antibacterial eye drops. If the problem is severe, it may require more intensive antibiotic or antifungal treatment to eliminate the infection, as well as steroid eye drops to reduce inflammation.
Dry Eye is a condition in which the eye produces fewer or lower quality tears and is unable to keep its surface lubricated. The main symptom of dry eye is usually a scratchy feeling or as if something is in your eye. Other symptoms include stinging or burning in the eye, episodes of excess tearing that follow periods of dryness, discharge from the eye, and pain and redness in the eye. Sometimes people with dry eye also feel as if their eyelids are very heavy or their vision is blurred.

A corneal dystrophy is a condition in which one or more parts of the cornea lose their normal clarity due to a buildup of material that clouds the cornea. These diseases:
Corneal dystrophies affect vision in different ways. Some cause severe visual impairment, while a few cause no vision problems and are only discovered during a routine eye exam. Other dystrophies may cause repeated episodes of pain without leading to permanent vision loss. Some of the most common corneal dystrophies include keratoconus, Fuchs’ dystrophy, lattice dystrophy, and map-dot-fingerprint dystrophy
Keratoconus is a progressive thinning of the cornea. It is the most common corneal dystrophy in the U.S., affecting one in every 2,000 Americans. It is most prevalent in teenagers and adults in their 20s. Keratoconus causes the middle of the cornea to thin, bulge outward, and form a rounded cone shape. This abnormal curvature of the cornea can cause double or blurred vision, nearsightedness, astigmatism, and increased sensitivity to light. The causes of keratoconus aren’t known, but research indicates it is most likely caused by a combination of genetic susceptibility along with environmental and hormonal influences. About 7 percent of those with the condition have a history of kerataconus in their family. Keratoconus is diagnosed with a slit-lamp exam. Your eye care professional will also measure the curvature of your cornea. Keratoconus usually affects both eyes. At first, the condition is corrected with glasses or soft contact lenses. As the disease progresses, you may need specially fitted contact lenses to correct the distortion of the cornea and provide better vision. In most cases, the cornea stabilizes after a few years without causing severe vision problems. A small number of people with keratoconus may develop severe corneal scarring or become unable to tolerate a contact lens. For these people, a corneal transplant may become necessary.
Fuchs’ Dystrophy is a slowly progressing disease that usually affects both eyes and is slightly more common in women than in men. It can cause your vision to gradually worsen over many years, but most people with Fuchs’ dystrophy won’t notice vision problems until they reach their 50s or 60s. Fuchs’ dystrophy is caused by the gradual deterioration of cells in the corneal endothelium; the causes aren’t well understood. Normally, these endothelial cells maintain a healthy balance of fluids within the cornea. Healthy endothelial cells prevent the cornea from swelling and keep the cornea clear. In Fuchs’ dystrophy, the endothelial cells slowly die off and cause fluid buildup and swelling within the cornea. The cornea thickens and vision becomes blurred. As the disease progresses, Fuchs’ dystrophy symptoms usually affect both eyes and include:
The first step in treating Fuchs’ dystrophy is to reduce the swelling with drops, ointments, or soft contact lenses. If you have severe disease, your eye care professional may suggest a corneal transplant.
Lattice Dystrophy gets its name from a characteristic lattice-like pattern of deposits in the stroma layer of the cornea. The deposits are made of amyloid, an abnormal protein fiber. Over time, the deposits increase and the lattice lines grow opaque, take over more of the stroma, and gradually converge to impair vision. Although lattice dystrophy can occur at any time in life, it most commonly begins in childhood between the ages of 2 and 7. In some people, amyloid deposits can accumulate under the epithelium of the cornea. This can erode the epithelium, and cause a condition known as recurrent epithelial erosion. This erosion alters the cornea’s normal curvature and causes temporary vision problems. It can also expose the nerves that line the cornea and cause severe pain. To ease this pain, an eye care professional may prescribe eye drops and ointments to reduce the friction of the eyelid against the cornea. In some cases, an eye patch may be used to immobilize the eyelid. The erosions usually heal within days, although you may have some pain for the next six to eight weeks. By age 40, some people with lattice dystrophy have scarring under the epithelium that can impact vision to such an extent that the most effective treatment will be a corneal transplant. Although the early results of corneal transplantation are typically good, lattice dystrophy may reappear later and require long-term treatment.
Map-Dot-Fingerprint Dystrophy, also known as epithelial basement membrane dystrophy, occurs when the basement membrane develops abnormally and forms folds in the tissue. The folds create gray shapes that look like continents on a map. There also may be clusters of opaque dots underneath or close to the map-like patches. Less frequently, the folds form concentric lines in the central cornea that resemble small fingerprints. Symptoms include blurred vision, pain in the morning that lessens during the day, sensitivity to light, excessive tearing, and a feeling that there’s something in the eye. Map-Dot-Fingerprint Dystrophy usually occurs in both eyes and affects adults between the ages of 40 and 70, although it can develop earlier in life. Typically, map-dot-fingerprint dystrophy will flare up now and then over the course of several years and then go away, without vision loss. Some people can have map-dot-fingerprint dystrophy but not experience any symptoms. Others with the disease will develop recurring epithelial erosions, in which the epithelium’s outermost layer rises slightly, exposing a small gap between the outermost layer and the rest of the cornea. These erosions alter the cornea’s normal curvature and cause blurred vision. They may also expose the nerve endings that line the tissue, resulting in moderate to severe pain over several days. The discomfort of epithelial erosions can be managed with topical lubricating eye drops and ointments. If drops or ointments don’t relieve the pain and discomfort, there are outpatient surgeries including:
Herpes Zoster (Shingles) is a reactivation of the varicel-la-zoster virus, the same virus that causes chickenpox. If you have had chickenpox, the virus can live on within your nerve cells for years after the sores have gone away. In some people, the varicel-la-zoster virus reactivates later in life, travels through the nerve fibers, and emerges in the cornea. If this happens, your eye care professional may prescribe oral anti-viral treatment to reduce the risk of inflammation and scarring in the cornea. Shingles can also cause decreased sensitivity in the cornea. Corneal problems may arise months after the shingles are gone from the rest of the body. If you experience shingles in your eye, or nose, or on your face, it’s important to have your eyes examined several months after the shingles have cleared.
Herpes of the eye, or Ocular Herpes, is a recurrent viral infection that is caused by the herpes simplex virus (HSV-1). This is the same virus that causes cold sores. Ocular herpes can also be caused by the sexually transmitted herpes simplex virus (HSV-2) that causes genital herpes. Ocular herpes can produce sores on the eyelid or surface of the cornea and over time the inflammation may spread deeper into the cornea and eye, and develop into a more severe infection called stromal keratitis. There is no cure for ocular herpes, but it can be controlled with antiviral drugs.
Iridocorneal Endothelial Syndrome (ICE) is more common in women and usually develops between ages 30-50. ICE has three main features:
ICE is usually present in only one eye. It is caused by the movement of endothelial cells from the cornea to the iris. This loss of cells from the cornea leads to corneal swelling and distortion of the iris and pupil. This cell movement also blocks the fluid outflow channels of the eye, which causes glaucoma. There is no treatment to stop the progression of ICE, but the glaucoma is treatable. If the cornea becomes so swollen that vision is significantly impaired, a corneal transplant may be necessary.
A Pterygium is a pinkish, triangular tissue growth on the cornea. Some pterygia (plural for pyterygium) grow slowly throughout a lifetime, while others stop growing. A pterygium rarely grows so large that it covers the pupil of the eye. Pterygia are more common in sunny climates and in adults 20-40 years of age. It’s unclear what causes pterygia. However, since people who develop pterygia usually have spent significant time outdoors, researchers believe chronic exposure to UV light from the sun may be a factor. To protect yourself from developing pterygia, wear sunglasses, or a wide-brimmed hat in places where the sunlight is strong. If you have one or more pterygia, lubricating eye drops may be recommended to reduce redness and soothe irritation. Because a pterygium is visible, some people might want to have it removed for cosmetic reasons. However, unless it affects vision, surgery to remove a pterygium is not recommended. Even if it is surgically removed, a pterygium may grow back, particularly if removed before age 40.
Stevens-Johnson Syndrome (SJS), also called erythema multiforme major, is a disorder of the skin that also affects the eyes. SJS is characterized by painful blisters on the skin and the mucous membranes of the mouth, throat, genitals, and eyelids. Often, SJS begins with flu-like symptoms, followed by a painful red or purplish rash of blisters that spread. SJS can cause severe conjunctivitis, iritis (an inflammation inside the eye), corneal blisters and erosions, and corneal holes. In some cases, SJS can lead to significant vision loss. The most commonly cited cause of SJS is an allergic reaction to a drug or medication, particularly sulfa drugs. It is also associated with viral infections. Treatment for the eye may include artificial tears or lubricating eye drops, antibiotics, or corticosteroids. About one third of those who develop SJS will have one or more episodes of the disease. SJS occurs twice as often in men as in women, and most often affects children and young adults under 30, although it can develop at any age.